Should You Take Testosterone? Symptoms, Pros / Cons, and What to Ask Your Doctor
Nov 11, 2025
In your 40s, 50s and beyond, if you're thinking hormones, you’re probably thinking about estrogen and progesterone—but don't forget testosterone: it matters for women, too. "Testosterone is just as important for health and vitality in women as estrogen," - that's from Dr Mary Claire Haver, a renown OB/Gyn Surgeon, Lecturer, best selling author and a top voice in Menopause & midlife care for women.
But it's frustrating, because this hormone is often overlooked in women’s mid-life care, even though it plays a real role in sexual health, mood, energy and more. Let’s explore how low testosterone shows up, what it can do for you when it's optimized, what the risks are, how it’s prescribed (and what to ask your doctor), and how this fits into navigating midlife optimally for you. (note: I am currently taking Hormone Replacement Therapy, and in addition to estradiol and progesterone, I also take Testosterone.)
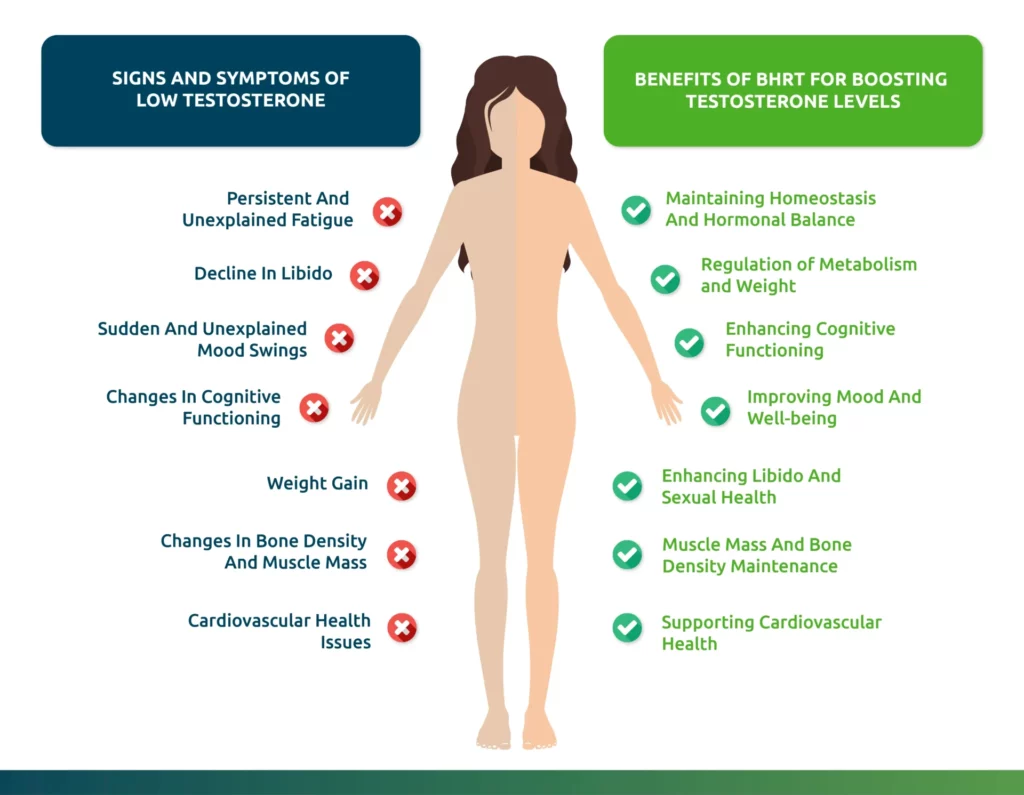
Signs & Symptoms of Low Testosterone in Midlife Women
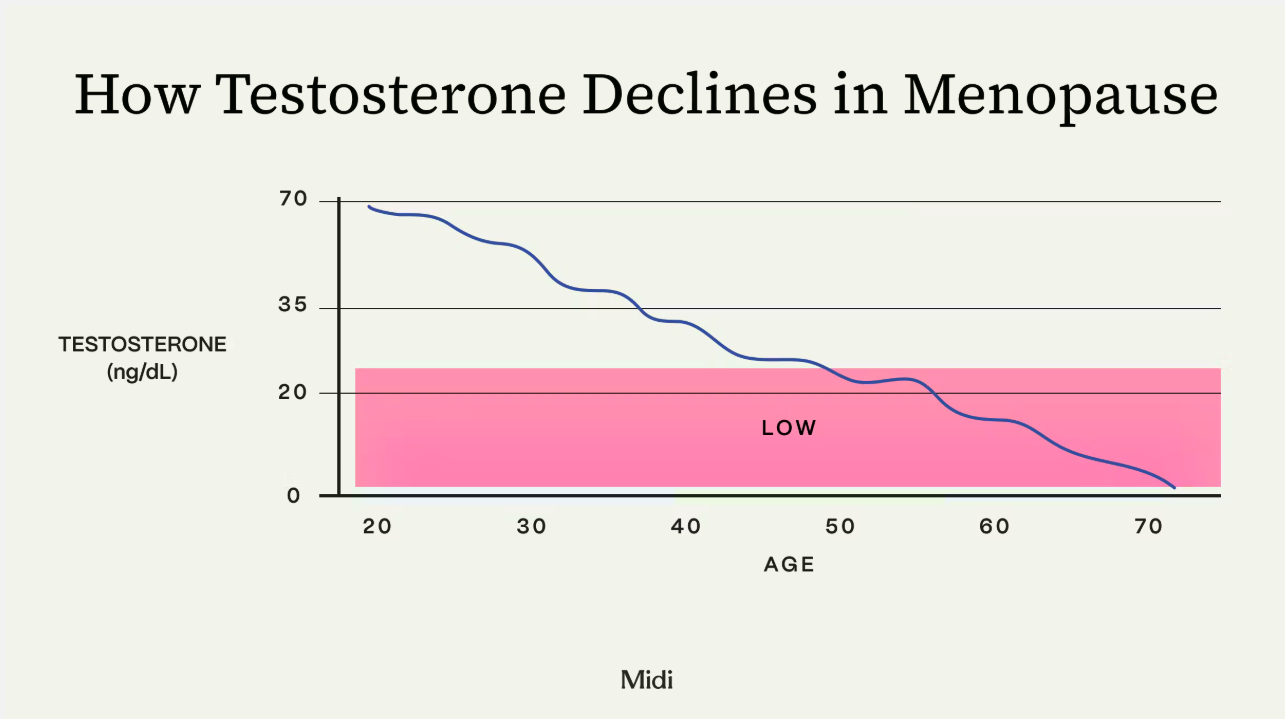
Because women’s testosterone levels are much lower than men’s, and because there is no standard FDA-approved “testosterone deficiency in women” threshold in the U.S., recognizing low Testosterone can be tricky. But many clinicians agree on a pattern of symptoms. (Dr. Haver notes the drop in Testosterone often coincides with perimenopause/menopause when ovaries and adrenals reduce output.)
Here are some symptoms you might relate to:
-
A drop in libido or sexual desire (especially if you are distressed by it)
-
Fewer sexual thoughts, less interest, less spontaneous desire
-
Decreased arousal or less satisfaction in intimate moments
-
Reduced energy levels, more fatigue, less “get up and go”
-
Loss of muscle mass or difficulty building/maintaining muscle
-
Increased fat around mid-section, slower metabolism (though many things influence this)
-
Mood changes: perhaps more brain fog, less motivation, more “meh” days
-
Possibly weaker bone/muscle support (since androgens play a role in bone and muscle health)
-
In some cases, genitourinary changes: some research links low Testosterone to bladder/vestibule issues, recurrent UTIs, and pain with intimacy.
If you’re thinking “Yep—I’ve got a few of these”, you’re not alone. And you definitely have the right to discuss this with your practitioner as part of your overall mid-life health.
What Testosterone Can Do for Women in Midlife
While clinical trials have not evaluated safety or efficacy of compounded testosterone for any indication (the funding for female midlife research has been woefully inadequate), here’s where testosterone (under proper medical supervision) is showing promise for women in midlife:
-
Improved sexual desire and satisfaction. Several studies in postmenopausal women show that testosterone therapy can improve libido and reduce distress around low desire. For instance, Dr. Rachel Rubin notes there is “global consensus” that Testosterone therapy improves libido in postmenopausal women with hypoactive sexual desire disorder (HSDD).
-
Better muscle/bone support. Because androgens influence muscle mass and bone strength, optimizing testosterone (in synergy with your strength training) could help you maintain lean muscle, bone density, and metabolic rate, all of which are crucial to helping you age optimally.
-
Energy, mood, and motivation. While the evidence is less robust, many women report better vitality and mood shifts when hormones are well-balanced (including testosterone).
-
Sexual/urogenital health. Testosterone may support tissues of the vulva, vagina, urethra, and bladder. For example, in women with genitourinary symptoms (pain with sex, recurrent UTIs, vestibulodynia) androgen-based therapies may play a role.
Important caveat: This is not a standalone miracle fix. It must be part of a broader strategy of sleep, movement, nutrition (hello, protein-forward meals and beauty superfoods!), stress management, and checking other hormonal systems. Dr. Haver emphasizes that Testosterone is part of the hormonal ecosystem (with estrogen, progesterone, adrenal health).
The Reality & Risks of Taking Testosterone
Because I like to be transparent with you and avoid over-hyped claims, let’s walk through the side-effects, regulatory gaps, and what to watch out for.
🔍 Regulatory status & dosing
-
In the U.S., there is no FDA-approved testosterone product specifically for women (again, the research funding gap is to blame). Many doctors use male-approved products off-label, or compounded formulations; as an example, this is what my hormone specialist and I have done.
-
Because of this, dosing must be handled carefully, ideally by someone experienced in female hormone therapy, and it must be titrated to lab results. One guideline suggests women may need about one-tenth of the standard male dose of a 1% transdermal testosterone gel to reach pre-menopausal female physiological range (this is what I use).
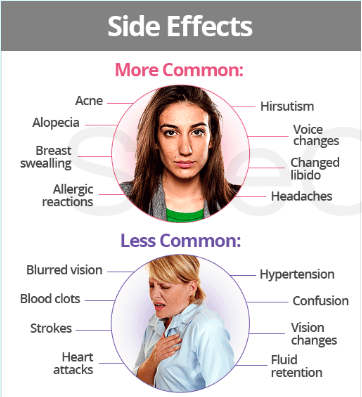
⚠️ Possible side-effects
Even with careful dosing, potential unwanted effects include:
-
Excess hair growth (hirsutism) or male-pattern hair changes
-
Acne or oiliness of skin
-
Deepening of the voice (rare but real)
-
Changes in cholesterol levels or lipids
-
Mood changes or irritability
-
Possibly changes in liver enzymes (depending on form)
-
Because of regulatory gaps and less long-term female data, any therapy should be monitored for safety. Dr. Haver highlights that while the data for sexual function is encouraging, “clinical trials have not evaluated safety or efficacy of compounded testosterone for any indication” in women.
🧬 What we don’t know (yet)
-
Long-term data (10-20 years) in women on testosterone is scarce.
-
Because there’s no dedicated FDA approved female testosterone product, much of the use is off-label.
-
The “right” testosterone level for a woman is not firmly established (Dr. Haver notes: “There is no testosterone level for diagnosis of HSDD or for use as a treatment target”). The 'Pause Life by Dr. Mary Claire Haver
-
Interactions with other hormones, medications, or underlying conditions need individualisation.
How Testosterone Therapy Is Prescribed & What to Ask Your Doctor
Here’s your practical checklist to bring into a doctor’s visit (and you know I love a checklist). Because you’re the empowered mid-life woman doing the research, and I'm here to help you.
🧪 Typical prescription workflow
-
Baseline evaluation
-
Ask for labs: total testosterone, SHBG (sex hormone-binding globulin), possibly free testosterone, estradiol, progesterone, DHEA, adrenal panel, thyroid.
-
Review symptoms: low libido, fatigue, mood, muscle loss, genitourinary symptoms.
-
Review other causes: thyroid issues, depression, medications, sleep apnoea, lifestyle.
-
Rule out contraindications (active hormone-sensitive cancers, severe liver disease, uncontrolled heart disease).
-
-
Choosing form and dose
-
Likely a low-dose transdermal testosterone gel or cream (off-label) or compounded preparation.
-
Start low, monitor levels and symptoms.
-
Dr. Rubin notes that for women, about one-tenth the male dose is a typical starting point.
-
-
Ongoing monitoring
-
Regular labs (maybe every 3-6 months) to track testosterone, lipids, liver enzymes, hemoglobin/haematocrit (though less of an issue than in men).
-
Monitor for side‐effects and adjust.
-
Continue your holistic plan: diet, strength training, sleep, stress management (so your muscle, metabolic and skin goals stay aligned).
-
❓ Questions You Should Ask Your Provider
-
“Why am I a good candidate for testosterone (vs focusing on other hormones or lifestyle)?”
-
“Given my age, health history and goals (for example: strength training, skin health, libido), what is the target testosterone level and how will you monitor it?”
-
“Which formulation are you suggesting (gel, cream, compounded) — what are the pros/cons in my case?”
-
“What dose will we start with, and what constitutes a safe upper limit for me?”
-
“What are the known risks or side-effects in women, and how will we mitigate them?”
-
“How will this interact with other hormones I’m on (estrogen, progesterone, thyroid, etc)?”
-
“How long will we trial it, and how will we decide if it’s ‘working’ for me?”
-
“What lifestyle or nutrition supports do you recommend alongside this so that I get the biggest benefit (and minimise side-effects)?”
How Testosterone Fits Into Your Bigger Picture of Aging (Well)
If you're like me, you're wanting to use Testosterone as a means to help optimize your life in midlife and beyond. But Testosterone isn't a magic pill; it's important to approach Testosterone as another “tool in your toolbox,” not the only one. It works best when combined with:
-
-
Enough high-quality protein (aim for ~120–130g/day) to support muscle synthesis.
-
Strength training + mobility + stability work, aka movement (I like to vary between all three of these for vitality, strength & flexibility). Hormones + training = synergy.

-
Adequate sleep (poor sleep disrupts hormone regulation)
-
Good nutrition (protein-forward meals, antioxidant-rich foods, anti-inflammatory eating)
-
Stress management (high cortisol can suppress sex hormones)
-
-
Stay realistic: Improvements may show up in libido, muscle and mood—but they don’t happen overnight, and optimizing hormone therapy is a process.
-
Keep a log of symptoms (libido, energy, mood, training performance) so you can objectively measure changes.
Personally, for me, adding Testosterone to my Hormone Replacement Therapy has yielded me lots of benefits. Not only has my libido improved, but I feel more spontaneous, energized and active throughout the day. I'm more motivated to do hard things that are beneficial for me that I don't like to do (like weight training or jumping into my cold plunge), I'm less fatigued and my mood is great.
I've done the risk analysis, and for me, Testosterone has made sense and I will continue to use it.
Final Thoughts
If you’re reading this and thinking “Yes — my body doesn’t feel like it used to, and I suspect hormones are involved,” this is your encouragement: you do have control (and knowledge) to ask greater questions, demand better answers, and partner proactively with your healthcare provider.
As Dr. Haver says: While aging is inevitable, suffering in silence is optional.
And Dr. Rubin reminds us: Your sexual health, your vitality, your sense of self matter — and hormone support (including testosterone) can be part of reclaiming that.
Let's do this, lovelies; let's age well naturally. 💪🌿
x
Juliana
PS - if you have questions? Or you enjoyed this blog post?? I love hearing from you! Drop me a note in the comments below and don't forget to👇 sign up for our monthly newsletter! 👇 Our monthly newsletter has all kinds of strategies on how to age well: nutrition, exercise, sleep, HRT, clean beauty, facial exercise & more. 💋