What I wish I'd known before starting HRT
Aug 24, 2025
I was recently talking to my friend Beth* about HRT, and she mentioned a less-than-stellar experience with her doctor, who begrudgingly put her on (the lowest dose) of hormones. After about six months of this dosage: while she doesn't feel great, she also doesn't feel terrible. But this feels like purgatory, and we really deserve better. We deserve to feel as good as possibly can. Right??
If you're thinking about hormone replacement therapy (HRT), my wish for you is to go into your doctor's meeting already informed about HRT, your symptoms and what you might need, so you aren't poorly treated like my friend, or gaslit about your symptoms being "all in your head."
Drawing on insights from experts like Dr. Peter Attia, Dr Rachel Rubin, Dr. Mary Claire Haver and my own personal HRT journey (which took 20ish months to finally get right), here’s what I wish someone told me before I started HRT (and I'm including some key files for you, like my 20 Questions to ask your Doctor, a Symptom Tracker, and a Provider Symptom Question Guide).

*not her real name
1. “It’s Not One Size Fits All”
The medical community likes easy. Your doctor typically only has 15 minutes to diagnose you and prescribe some course of treatment, so if you could kindly fit your symptomology into a nice prescriptive box so the right medication and dosing solution is obvious, that would be perfect.
But perimenopause is anything but prescriptive. Perimenopause - and its symptoms - differ dramatically from woman to woman. At 54, I'm still perimenopausal, but I know women who reached menopause in their early 40s. And I have a friend who was still in perimenopause at 57. I don't have hot flashes, but my insomnia and joint pain were debilitating. Others suffer from depression, anxiety and mood swings. Weight gain. Bloating. Cracked Heels. Tinnitus. I could go on and on (there are more than 100 different types of symptoms).
So it makes sense that your HRT dose and prescription needs to be unique to you. Dr. Peter Attia emphasizes that the right regimen hangs on three dynamic factors: what your labs are saying, how severe your symptoms are, and how your body changes / adapts as you traverse perimenopause.
You need to factor in that while you're in perimenopause, your body will still be trying to produce hormones - and that sometimes it will succeed, creating periods of spiking estrogen and then tanking levels. This matters because getting your hormones "balanced" while in perimenopause is a little like putting the wings on an aircraft while it's in mid-flight: more art-than-science, with lots of paying attention to symptoms rising and subsiding, and titrating your dosage until you feel better.
Again - wouldn't it be nice to be prescriptive? But that's not perimenopause. You're on a journey, and at the end, it'll all be worth it once the night sweats, brain fog and joint pain subside.

I've learned to expect some periods of of bloating, water retention, or mood fluctuations tied to estrogen spikes or progesterone lows, and to not freak out - I haven't just gained 6 pounds over 2 days - but that it's my hormones doing their thing, they'll calm down in a minute. The best thing I can do is stay the course with daily exercise / movement, nutrition, sleep prioritization and limiting alcohol. I trust my body to come back into alignment - and it always does.
2. Titrate as Necessary
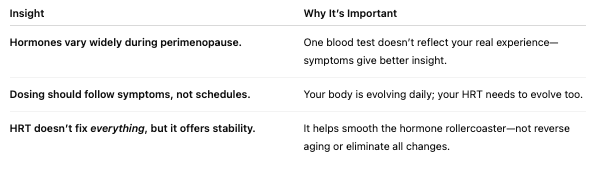
Again, it would be so nice if HRT were a one-size-fits-all: just take some hormones and poof!: you're feeling like you're in your 20s! But it's not like that. Dr. Mary Claire Haver vividly describes perimenopause as a hormone rollercoaster—a period marked by unpredictable spikes and dips in estrogen and progesterone. Hormone levels (like estradiol and FSH) can go from normal to abnormal within 24 hours. It's hard to pinpoint the accurate dosing for you at your exact moment in perimenopause. And just when you've got it figured out - your levels will likely change again.
Bloodwork is useful - but just as a marker at that point in time. Traditional blood tests just capture one moment in time, so they don't reflect this day-to-day volatility. So it's super-important that your hormone therapy be based on your symptoms, and that it be dynamic, personalized and responsive.
In other words: your therapy should be adjusted based on symptoms such as sleeplessness, anxiety, bloating, or mood swings, not just lab values.
Practical Next Steps You Can Take:
- Track symptoms consistently—use a symptom tracker to notice triggers, patterns, and improvements. I've included one for you to download, at the end of this article.
- Share regular updates with your provider, not just labs. If I'm not feeling right, I call and let my doctor know and usually within 24 hours, we're adjusting my hormone therapy to bring me back into balance.
- Ask: “Should we adjust based on these symptoms?”—especially when sleep, mood, or bloating shifts.
- Work with someone who treats hormone care as dynamic. This last point is so important! If your doctor has the one-size-fits-all approach, you might wind up like my friend Beth. My questionnaire to ask your doctor screens for this, and gives you insight into your hormone specialist and if she's willing to work with you to titrate your therapy until you're feeling better.
3. Diet Can Mitigate a lot of Symptoms
The bad news: you don't feel like yourself. The good news: you can do SO MUCH to change that. One of the biggest levers you can pull to feel better quickly is focusing on what's at the end of your fork.
Nutrition is foundational to hormone stability. Dr. Peter Attia stresses that focusing on long-term metabolic health, rather than trending diets, is key to managing midlife hormone shifts. By stabilizing insulin, supporting cardiovascular resilience, and building lean muscle, you're setting the best possible stage for hormone modulation and minimizing common symptoms like weight gain, mood swings, and fatigue.
In other words: choose your hard. Breaking up with processed foods and added sugars is hard, but what's also hard: night sweats, brain fog, depression & anxiety, joint pain, heart palpitations, weight gain and ... you know.
And one of the sneakiest things that makes perimenopause brain fog worse? Added sugar. As estrogen drops, your brain becomes more sensitive to blood sugar spikes and crashes — which means that muffin or candy bar can leave you feeling foggy, forgetful, and drained. Research shows that high-sugar diets are tied to poorer focus and memory, while balanced blood sugar is linked to fewer hot flashes, better sleep, and clearer thinking.

So what to eat? You want to prioritize protein and fiber, aiming to get about 1 gram of protein per pound of your ideal body weight, and about 25 grams of fiber daily. Minimize added sugars and avoid highly refined carbs (I cut my sugar cravings by swapping out sweets for dates and fresh fruit, which offset any sugar they have with fiber).
Focus on meals and snacks that pair protein, fiber, and healthy fats to keep glucose steady, like Greek yogurt with berries instead of a pastry, or roasted chickpeas instead of chips. Cut out high processed foods and alcohol. Eat healthy foods that are real, unprocessed and optimally designed to help you thrive and your body will respond in spades. I wrote a recent blog post about how I did a total reset, this might help you as well.
4. Exercise Can Make You Feel Better
I can't say it enough: exercise -- weightlifting, mobility, stability (my holy trinity) are essential for your overall well being during perimenopause and beyond. I know it's hard when you're feeling fatigued and exhausted from the insomnia - I've been there! But exercise is a critical, non-negotiable factor when it comes to navigating perimenopause. It seems counter-intuitive but you'll feel better because of exercise, and your symptoms will dissipate. You'll feel stronger, your sleep quality will improve, your mood will stabilize, and you'll have more energy.
More than that, Dr. Haver warns that 85% of women experience new joint or musculoskeletal pain during perimenopause, even without injury—pain that can be debilitating for about 20% of women. And while hormone therapy can help, exercising and strengthening your joints - along with stability work - is equally vital for maintaining joint function, reducing pain, and building physical resilience. It's really use it or lose it.
How to approach exercise in perimenopause? Here's what I do:
- I start every morning with a stretching routine that brings my body into alignment, strengthens my back, legs and knees and gets the stiffness out of my body;
- I strength-train 2-3x / week (max 1-hour sessions, most of them are closer to 45 minutes), with the intent to meet my prior strength goals or do progressive overload;
- I'll do a stability workout or mobility work on the days I'm not lifting;
- I incorporate daily walks throughout my day (my doggo needs to do her business) so that I get between 7 - 10K steps / day;
- I squeeze in a humbling karate class 1-2x / week to round things out.
My goal is to do daily movement. I find that even a modest amount of weight lifting / mobility / stability work - (as little as 15-20 minutes a day) helps me feel better than taking a rest day. It dramatically improves my mood, how I feel in my body, and my sleep.
Another great hack I use is my weighted vest. A weighted vest is such a great way to stimulate bone stress and bone density—and we know those take a negative turn when estrogen leaves the building, accelerating bone loss in perimenopause and beyond. It’s a practical, low-barrier method to strengthen both bone and muscle in daily movement and I try to walk with it as often as I can. You can shop my recommended weighted vest here.
5. You Are Your Own Primary Care Provider
Until our medical system improves and prioritizes women beyond our childbearing years, my experience has shown me that you are your own primary care doctor when it comes to navigating perimenopause and HRT. You’re the one living in your body every single day. No lab coat, however well-meaning, has to contend with your hot flashes at 3 a.m., the brain fog that derails your thoughts, or the crippling anxiety. Sadly, it's alllll too common: a woman experiences confounding symptoms and finally goes to her doctor, only to be misled by a misinformed-but-well-intending doctor who hasn't studied the midlife transition and is dismissive about symptomology or HRT protocols. Leaving her frustrated and dismissed. It's not all in your head. You deserve better.
That’s why you have to advocate for yourself and find the right provider. Screening a doctor or nurse practitioner before you commit is crucial. Use a guide like my “20 Questions to Ask Your Provider About HRT” and bring it with you to your appointment. If your provider bristles at your curiosity or dismisses you, that’s a BIG red flag. Is HRT right for you? A good clinician will welcome your questions, explain their reasoning, and work with you based on your symptoms—not just a one-time lab result.
Getting informed is also part of reclaiming your power. One of the best resources I recommend is The New Menopause by Dr. Mary Claire Haver. She does an incredible job unpacking the science in a way that’s approachable, and she gives women the tools to understand what’s happening in their bodies. Reading books like hers arms you with knowledge so you can advocate for yourself with confidence instead of uncertainty and deflate gaslighting.
Also, we live in the information age. Become familiar with ChatGPT and research your symptoms. Talk to your girlfriends. Follow women your age who are navigating perimenopause and seem to be doing it well - gather their information and advice as part of your perimenopause toolkit.
And don’t underestimate the power of learning from experts who are active in the perimenopause space on social media. Physicians like Dr. Mary Claire Haver, Dr. Rachel Rubin, and Dr. Jen Gunter, as well as longevity experts like Dr. Peter Attia, share ongoing insights that can help you connect the dots between symptoms, lifestyle, and medical options. While not every TikTok or Instagram post is gold, following credible experts helps you stay in the loop with the latest conversations about HRT, bone health, cardiovascular risks, and symptom management.
The bottom line? You’re not being “difficult” by asking questions or seeking second opinions. You’re being responsible. Perimenopause is too important to navigate passively—you deserve providers who respect your voice, resources that make you feel informed, and a plan that reflects your unique needs. So don’t hand over your power. Carefully select your care team, stay on top of your symptoms, and keep your hands on the wheel of your own health journey until you feel better - trust, it's worth it.
Let's age well naturally, lovelies-
x
Juliana
PS - if you enjoyed this blog post, sign up for our monthly newsletter! We drop aging well strategies on nutrition, exercise, sleep, HRT, clean beauty, facial exercise & more.